Congenital Hypothyroidism
Congenital Hypothyroidism Introduction
Congenital hypothyroidism is a condition in which children are born with an inability to make adequate amounts of thyroid hormones. Thyroid hormones are necessary for normal brain growth during the first 3 years of life. Therefore, proper treatment of children with congenital hypothyroidism must be started as soon as possible after birth in order to ensure normal brain growth and development.
In the past, many children with congenital hypothyroidism were not diagnosed early enough and their brain development was already abnormal by the time treatment was started. Over the past few years, babies born in the USA have had their thyroid hormone levels checked soon after birth so that children with congenital hypothyroidism can be promptly detected and treated. This pamphlet answers a few of the more common questions about congenital hypothyroidism.
What are thyroid hormones?
Thyroid hormones are produced by the thyroid gland, which is usually located in the front of the neck. The main type of thyroid hormone is called T4. The thyroid gland releases T4 into the bloodstream. Most of the T4 in the blood is stuck onto a protein in the bloodstream called thyroid binding globulin (TBG), while the rest of the T4 floats freely in the blood, and is called free T4. It is not known why we have two forms of T4 in the body, because only free T4 is important for promotion of growth, development, and bodily function.
What is congenital hypothyroidism?
Congenital hypothyroidism is a condition in which a child is born with an inability to make adequate amounts of thyroid hormones. “Congenital” refers to something that you are born with. “Hypothyroidism” means low thyroid hormone levels.
What causes congenital hypothyroidism?
There are many things that can cause congenital hypothyroidism. In the old days, a deficiency of iodine before or after birth could cause hypothyroidism. This is because iodine is a key ingredient in the production of thyroid hormones. This form of congenital hypothyroidism is still common in some parts of the world. However, it is very uncommon in the USA since our modern diet provides adequate amounts of iodine.
The most common cause for congenital hypothyroidism in the USA today is a malformation of the thyroid gland. The development of the thyroid gland 2occurs before birth and is a very complicated process. If any part of the process is not right, the thyroid gland will not function properly after birth. Some children with congenital hypothyroidism are born without a thyroid gland; others are born with only part of the gland, or the gland doesn’t develop in the right place. We do not completely understand what causes this malformation to occur. This type of congenital hypothyroidism usually does NOT run in families.
Very rarely, congenital hypothyroidism can be due to a disorder in which the thyroid gland is present but lacks the ability to manufacture thyroid hormones. This type of problem tends to run in families.
How common is congenital hypothyroidism?
In the USA, about 1:4000 children are born with congenital hypothyroidism.
What is TSH?
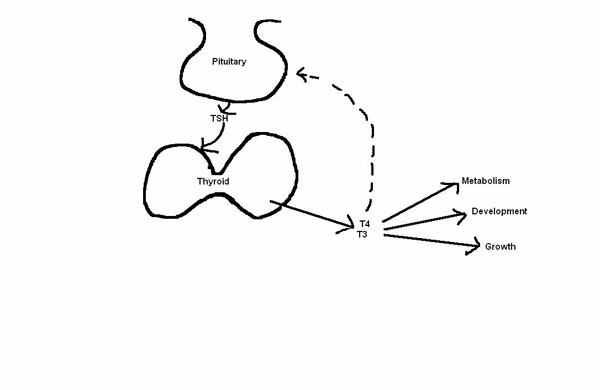
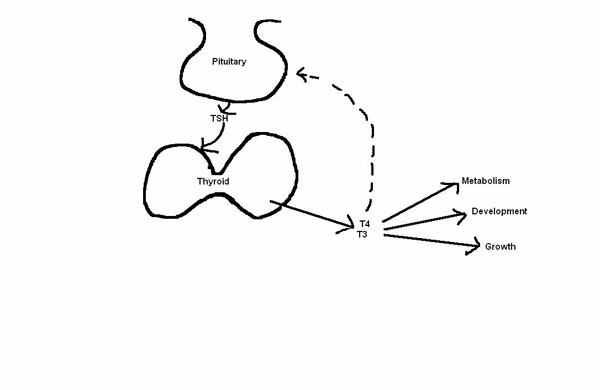
TSH stands for thyroid stimulating hormone. TSH is produced by the pituitary gland in the brain, released into the bloodstream, and travels to the thyroid gland where it stimulates the production of thyroid hormones. If the thyroid gland is malformed and not working properly, the pituitary gland senses the lack of thyroid hormone in the blood, and produces extra amounts of TSH in an effort to make the thyroid work properly. In most cases of congenital hypothyroidism, the thyroid gland cannot respond to the extra TSH. The TSH levels then become very high.
In very rare cases, the congenital hypothyroidism can be due to a deficiency in TSH production by the pituitary gland. In these cases, the thyroid gland is normally formed but cannot function because of the lack of simulation by TSH. Most of these babies also have other problems with the pituitary gland, and many of them are very sick shortly after birth.
What happens if congential hypothyroidism is not treated?
One of the main things the thyroid hormones do is to control the pace at which the body functions. If thyroid hormone levels are low, the body tends to slow down all of it’s functions. Some babies with congenital hypothyroidism have problems right after birth such as constipation, swelling of the tongue and other body parts, and poor feeding. Most babies with unrecognized congenital hypothyroidism seem to be normal at birth and only later develop problems such as abnormally slow growth and development of teeth, and very weak muscles. In severe cases, the brain does not develop normally and the child will be mentally retarded.
Does the treatment work?
Hundreds of children with congenital hypothyroidism have now been detected and treated early due to the newborn blood testing program. The children who receive early treatment and who continue to receive proper treatment have normal growth and development. Children who are not treated early enough or who do not receive the proper amount of medication may grow and develop at an abnormally slow rate.
How is treatment monitored?
At each visit, blood is taken and sent to the laboratory for measurement of thyroid hormones. We usually check the level of total T4 and free T4. At the same time, we measure TSH. Because the pituitary is able to sense the level of T4 any increase in the level of TSH indicates that the amount of T4 in the blood is inadequate. The pituitary is not able to sense whether the T4 is coming from the thyroid gland or from the thyroid tablets your child is taking.
How often shoud blood tests for thyroid hormone be checked?
To make sure that a child is receiving the proper amount of the thyroid medication, a blood test is usually taken about 4-6 weeks after the first dose is given. T4 and TSH levels are measured in this sample. Some laboratories are also able to measure free T4. Once the right dose is established, blood levels of these hormones should be checked about every 3 months until the age of 3 years. This is to make sure that the levels remain normal for the entire period during which the brain is developing. After the age of 3 years, the testing can be performed every 4-6 months. As a child grows, the dose of the thyroid medication needs to be gradually increased according to the laboratory test results and the child’s growth measurements.
How long will the thyroid medication be needed?
Congenital hypothyroidism is almost always a life-long condition, and treatment is required throughout life. Even after the brain has stopped developing, thyroid hormone is necessary for normal growth, normal energy levels, and normal sexual development and functioning. Older children with congenital hypothyroidism can be very short, perform poorly in school, and have very late puberty if they are not treated. Adults with untreated hypothyroidism can be very lazy, mentally slow, and overweight. Severe hypothyroidism in either children or adults can lead to very thin and fragile hair, partial baldness, very dry skin, and an increased cholesterol.
In very rare cases, congenital hypothyroidism can be temporary. In these cases, a child will have normal T4 and TSH levels throughout the first 3 years of life without any changes in the dose of thyroid medication. If this happens, the doctor may recommend a 4-6 week period without thyroid medication after the age of 3 years to see whether the medicine is still needed.
How often will my child need to see the doctor?
Your child should see his/her pediatrician or family doctor on the same schedule as for other children for checkups, illnesses, and shots. If your child has congenital hypothyroidism, he/she should visit a pediatric endocrinologist at least every 3 months during the first 3 years of life, and about every 4-6 months after that until he/she has finished growing and developing. A pediatric endocrinologist is a specialist in childhood hormone disorders. These visits are recommended to make sure that the thyroid hormone therapy is adequate.
Will my child’s brain development be normal?
If treatment is started before one month of age, there is every anticipation that your child’s development will be normal. However, your child’s development will need to be monitored regularly by your pediatrician. We recommend that a formal developmental assessment be made at 5 years of age before entry into kindergarten. These measures are to ensure that, if there are any learning disabilities or problems with speech or coordination, your can receive expert assistance to allow him/her to overcome them.
Hyperthyroid
What is the thyroid gland?
The thyroid gland is a butterfly-shaped structure that is located in the neck in front of the windpipe. When the thyroid gland enlarges, it can be felt (and sometimes seen) on either side of the throat, especially when a person swallows. The thyroid gland makes two hormones – thyroxine (T4) and triiodothyronine (T3). The thyroid hormones are important for several reasons: 1) Thyroid hormones affect body metabolism, or the way the body uses food for heat production and energy; 2) Thyroid hormones are necessary for proper growth in children; 3) Thyroid hormones are required for the proper development of the brain during infancy; and 4) Thyroid hormones affect the heart’s performance.
The thyroid gland produces the thyroid hormones under the direction and regulation of another hormone, thyroid stimulating hormone or TSH. The TSH is made by a gland in the brain called the pituitary. When the pituitary gland thinks the body needs more thyroid hormones, it releases TSH which stimulates the thyroid gland to make the thyroid hormones. When the pituitary gland the body has plenty of thyroid hormones, it slows down the release of TSH, and this then reduces the amount of thyroid hormones made by the thyroid gland. If this sounds complicated, think of the thyroid gland as the furnace in your house, and the pituitary gland as the thermostat that senses the room temperature and controls the heat production of your furnace.
What is hyperthyroidism?
Hyperthyroidism is a state in which thyroid hormones are overproduced. In hyperthyroidism, the T3 and T4 levels are too high. This overproduction of thyroid hormones causes weight loss, rapid heart rate, muscle weakness, increased sweating, intolerance of heat, sleep disturbances, irritability, moodiness, increased bowel movements, menstrual irregularity, and rapid speech. If allowed to progress, it may result in heart failure.
What is Graves’ Disease?
Graves’ Disease is the most common cause of hyperthyroidism and is usually associated with an enlarged thyroid gland, prominent eyes, and muscle weakness. It was first described by Dr. R.J. Graves in 1835.
What causes Graves’ Disease?
Graves’ Disease is caused by an abnormality in the immune system. (This is explained in the section below.) Often this abnormality affects more than one member in an extended family; this suggests that there may be an inherited tendency for some people to get Graves’ Disease.
Immune system problems: All healthy people have the ability to make antibodies to germs when they get sick. Antibodies recognize the germs as being foreign and act like “Packman” by gobbling up the germs and destroying them. But, sometimes the body gets confused and makes antibodies that look upon the thyroid gland as if it were a foreign germ. Some of these antibodies stimulate the thyroid gland; they’re called thyroid stimulating immunoglobulins (TSI). Some of the antibodies destroy the thyroid gland as if it were a germ; these are called ATA or anti-thyroid antibodies. Other antibodies block the normal production of the thyroid gland; these are called thyroid-blocking inhibitory immunoglobulins or TBI.
The severity of Graves’ Disease depends on which of these “confused” antibodies is being made. The body also may make antibodies to the muscles behind the eyes. This leads to an inflammation of the eye muscles and causes the muscles to swell and push the eye forward.
Once a child or adult develops Graves’ Disease, the immune system abnormality is present for life. There may be periods of rest when the disease is inactive (remission), and there may be other times when the disease is reactivated (relapse). At the present time, there are no treatments that will cure this immune system abnormality.
The immune system abnormality is usually just limited to antibodies that affect the thyroid gland and the eye muscles. The rest of the immune system is all right, and it is able to make normal antibodies that fight infection.
Graves’ Disease can begin anytime during life. Graves’ Disease, at different stages of life, is discussed below.
Newborn Hyperthyroidism
Infants born to mothers who have Graves’ Disease may be exposed during pregnancy to thyroid-stimulating antibodies (TSI) that cross the placenta. These antibodies produce hyperthyroidism in the baby by crossing the placenta and stimulating the baby’s thyroid. These infants may be born small and have weak muscles, rapid heart rate, fever, jaundice, breathing problems, enlarged thyroid glands, and prominent eyes. It may progress to irritability, feeding difficulty, sweating, weight loss, and frequent bowel movements. Newborn hyperthyroidism usually needs to be evaluated and treated promptly with medication to normalize the thyroid hormone levels. Fortunately, this type of hyperthyroidism usually resolves in 4-12 weeks when the mother’s thyroid stimulating antibodies disappear from the baby’s blood. Once this resolves, it is unlikely to recur.
Acquired Hyperthyroidism
Older children can develop hyperthyroidism for reasons that are not entirely understood. Girls are affected much more frequently than boys. Refer to the explanation of antibodies (above) to understand how older children develop hyperthyroidism.
Other Causes of Hyperthyroidism
Hyperthyroidism also can develop if a person eats food that is contaminated by thyroid hormones, or if a person takes in excessive amounts of iodine. People who normally take thyroid hormone medication to treat HYPOthyroidism (underactivity of the thyroid gland) can develop signs of HYPERthyroidism if they take too much thyroid medicine. Occasionally, benign (noncancerous) thyroid tumors and, occasionally, a short, intense infection or inflammation of the thyroid gland can cause hyperthyroidism.
What tests are commonly used to diagnose hyperthyroidism?
Hyperthyroidism usually is easily diagnosed by learning about the child’s symptoms and by giving the child a thorough physical examination. The tests that are explained below are used to judge the severity of the disease.
BLOOD TESTS
Thyroid hormone levels: The blood test may measure different forms of thyroid hormone – T4, T3 uptake, T3, Free T4 and TSH. TSI – thyroid stimulating immunoglobulins – used to detect Graves’ Disease in newborns.
THYROID IMAGING
To estimate the size and shape of the internal parts of the thyroid gland, your child’s doctor may order thyroid imaging tests. Your child may receive radioactive iodine orally or another radioactive substance through an IV (thyroid scan). These radioactive substances are concentrated in the thyroid gland, making is visible to the scanner. A picture is then taken which represents the size of the thyroid gland and locates obvious abnormalities. A technetium scan can be performed shortly after the child takes the medicine. With the radioiodine scan, there is a time lag between when the child takes the medicine and when the scan can be done.
PREGNANCY TESTS
Pregnancy tests are done routinely before thyroid scans are performed. This is because the radioactive substances used for scanning can cross the placenta and harm the baby.
Why treat hyperthyroidism?
Hyperthyroidism requires treatment to prevent dangerous weight loss, to prevent heart disease that can develop, to restore normal muscle tone and strength, and to prevent death.
How is hyperthyroidism treated?
Several treatment options are available. The endocrinologist will discuss each option with you, pointing out the advantages and disadvantages of each treatment option. Be sure to ask plenty of questions until you feel you thoroughly understand all the options.
MEDICATION
Propylthiouracil (PTU) or Methimazole can be taken orally several times a day to treat hyperthyroidism. These two medications block the thyroid gland’s ability to make the thyroid hormones. Of the various treatment options available, these medications are the only option that does not destroy the thyroid gland. This treatment is generally safe and highly effective. However, there are some problems connected with taking PTU or Methimazole.
- These medicines must be taken several times a day for at least two years.
- The relapse rate is high; that is, in 60-75% of cases, the hyperthyroidism may come back after the medications are stopped.
- There are possible side affects – skin rash (5% of cases), joint pains, liver problems, and agranulocytosis (not enough white blood cells to fight infections). Agranulocytosis is the most serious complication, and it occurs in about 5:1000 of people taking these medications. If a child taking either of these medications develops a persistent sore throat and fever, the medications are stopped and antibiotics are given. These complications are usually reversible when the medications are stopped but, occasionally, the outcome may be fatal.
NOTE: Regardless of the therapy option chosen, all children are first treated with one of these medications to normalize the thyroid hormone levels in the body.
Radioactive Iodine THERAPY
Using radioactive iodine, a nuclear medicine specialist destroys the overactive thyroid gland. First the child is treated with the anti-thyroid medication, then a test is done to determine the thyroid’s uptake of radioiodine and a scan is done to calculate the dose needed to destroy the thyroid gland. Finally, the radio-iodine is swallowed and the thyroid gland deteriorates.
The advantage of this treatment option is that it provides a relatively easy solution to the problem of having hyperthyroidism without the risk associated with having surgery.
Potential problems that should be considered are:
- Although radioactive iodine has been the preferred treatment in adults for a long time, pediatric endocrinologists used to be hesitant about using this treatment in children. This was because we did not have any long-term experience using radioactive iodine in children, and we worried that children might be prone to developing cancer in the remaining thyroid tissue. Now, after 30 years of using radioactive iodine in children, we have follow-up information from children treated at the Cleveland Clinic; those individuals who were treated as children with radioactive iodine for hyperthyroidism have had no increased occurrence of thyroid cancer. Similar follow-up information from Sweden also has confirmed that there is no increased occurrence of thyroid cancer in individuals treated with radioactive iodine therapy. Thus, our previous worries about the safety of radioactive iodine therapy in children seem to have been unfounded.
- There also was a theoretical concern about the possible association between radioactive iodine therapy and the development of leukemia, a cancer of the blood. Information from adults treated with radioactive iodine, as well as from children treated over the last 30 years has not revealed any increased occurrence of leukemia.
- There was concern that radioactive iodine might affect the testicles and ovaries of children, leading to malformations in their future children. These worries also have been unfounded; there has not been any increased occurrence of birth defects in the babies of adults treated as children with radioactive iodine. However, we must caution that if radioactive iodine is taken during pregnancy, there may be serious problems in the baby. Therefore, it is routine to perform a pregnancy test in all females before giving radioactive iodine therapy. NOTE: These risks may be discussed with the nuclear medicine specialist before you sign consent for this treatment option. You are encouraged to ask questions.
- The thyroid gland usually is destroyed totally by radioactive iodine treatment. Then the body cannot make thyroid hormone, and the person must take life-long daily thyroid medicine (pills). This eventually occurs in almost all patients.
SURGERY
The overactive lobe(s) of the thyroid gland can be removed surgically following a few weeks of taking the anti-thyroid medications listed above. The advantage of surgical treatment is that it offers a relatively quick solution to the problem of having hyperthyroidism, i.e., there are no longterm medication schedules to follow. However, there are problems connected with this option.
- Surgery requires several days in the hospital and is uncomfortable. Excessive bleeding, infection, and paralysis of the vocal cords can occur with thyroid surgery. Also, other glands that are located in the neck (parathyroid glands) can be damaged leading to problems with calcium regulation. One of these problems may occur in 1% of cases.
- It is quite likely that too much of the thyroid gland will be removed, and thyroid hormone tablets will have to be taken daily for life.
- If too little thyroid glandular tissue is taken out, you will again need to consider the treatment choices: radioactive iodine therapy, repeat surgery (difficult), and medication.
OTHER MEDICINE THAT MAY BE PRESCRIBED
To control the rapid heart rate and high blood pressure that may be present, your child’s doctor may prescribe propranolol [Inderal] or atenolol [Tenormin] for a brief period of time. This medicine should not be taken by children with asthma; please tell your doctor if your child has ever had wheezing episodes. It is important not to exercise while taking propranolol, as this may strain the heart.
Other Problems Associated with Hyperthyroidism
WEIGHT CHANGES
When hyperthyroidism is untreated, the body’s metabolic rate is very high. During this period, a person can eat an incredible amount of food and usually not gain weight. However, once treatment for the hyperthyroidism has begun and the blood thyroid levels return to normal, the body’s metabolic rate decreases. If the person continues to eat voraciously, rapid weight gain occurs. This can be quite a problem, especially for adolescents. You may want to meet with our dietitian before and during treatment of the hyperthyroidism to learn ways of coping with this change in body metabolism.
SCHOOL PROBLEMS
Children with hyperthyroidism cannot concentrate on schoolwork, and their irritability can interfere with normal student-to-student and student-toteacher relationships. We suggest you talk with your child’s teacher and school nurse about the effects that hyperthyroidism has on children’s behavior. Explain to the school personnel that, with proper treatment, your child’s thyroid levels will return to normal and that his/her behavior also will improve.
EYE PROBLEMS
If the hyperthyroidism has caused the eyes to bulge, the eyelids may not close completely. To keep the eyes moist during sleep, you may need to put lubricating eye drops in your child’s eyes at bedtime. None of the treatment options listed above cures the eye disease. However, the bulging eye problem may eventually resolve.
HYPOthyroidism
The thyroid gland may eventually “burn out” and stop making thyroid hormone. For this reason, your child will need to be checked every year for signs of HYPOthyroidism. When your child is an adult, he/she will need to see an adult doctor for this yearly checkup.
Graves’ Disease and Pregnanacy
Because of the effects of Graves’ Disease on you and your baby, we recommend that you plan your pregnancy and talk things over with your endocrinologist before you become pregnant. In addition to your usual obstetric care with your obstetrician, you will need to be monitored by your endocrinologist throughout the pregnancy. Even if you no longer have your thyroid gland because it was destroyed by radioactive iodine or surgery, you will still need to be cared for by your endocrinologist because your immune system may continue making TSI that can cross the placenta and affect your baby’s thyroid. If you are treated properly during your pregnancy, you can ensure your well-being and that of your baby.
Aquired Hypothyroidism
What is Acquired Hypothyroidism?
Hypothyroidism results from the inability of the body to produce thyroid hormones. These hormones act as chemical messengers to control growth and development of the body and brain, influencing energy use (metabolism), and direct the function of the heart, liver, kidneys and skin. “Acquired” means that it occurred sometimes after birth, when the thyroid gland was fully developed, and “Hypothyroidism” means low thyroid hormone levels.
What are thyroid hormones?
Thyroid hormones are produced by the thyroid gland. It is shaped like a bow tie or a butterfly and is usually located in the front of the neck, just below the “Adam’s apple”. The thyroid gland makes two hormones – thyroxine (T4) and triiodothyronine (T3). The thyroid hormones are important for several reasons: 1) they affect body metabolism, or the way the body uses food for heat production and energy; 2) they are necessary for proper growth in children; 3) they are required for the proper development of the brain during infancy; and 4) they affect the heart’s performance.
The thyroid gland produces these hormones under the direction and regulation of another hormone, thyroid stimulating hormone (TSH). The TSH is made by a gland in the brain called the pituitary. When the pituitary gland thinks the body needs more thyroid hormone, it releases TSH, which stimulates the thyroid gland to make the thyroid hormone. When the pituitary gland thinks the body has plenty of thyroid hormones, it slows down the release of TSH, and this then reduces the amount of thyroid hormones made by the thyroid gland. If this sounds complicated, think of the thyroid gland as the furnace in your house, and the pituitary gland as the thermostat that senses the room temperature and controls the heat production of your furnace.
What causes acquired hypothyroidism?
Typically, hypothyroidism is caused by an abnormality in the immune system, whereby antibodies fail to recognize the thyroid cells as part of your self. Therefore, the immune system produces antibodies that are directed against one’s own thyroid cell. This results in a chronic inflammation within the gland, causing enlargement of the gland. It also becomes firmer than normal and typically feels quite lumpy on careful examination. The chronic inflammation and antibodies gradually destroy the thyroid cells, resulting in hypothyroidism. In some cases, the chronic inflammation progresses to fibrosis and scarring, eventually resulting in the gland shrinking down and “melting away”. Usually, an abnormality of the immune system that results in damage or destruction of the thyroid gland causes acquired hypothyroidism. This process can cause loss of thyroid tissue or enlargement of the thyroid gland. The massive enlargement of the thyroid gland is sometimes referred to as a goiter. Other causes of hypothyroidism include surgical removal of the gland or radiation to the gland. Occasionally, the disease does not involve the thyroid gland itself, but is located within the pituitary gland or the area of the brain just above it, called the hypothalamus. Hypothalamic or pituitary disease, such as a cyst, a growth, 3 surgery to that area of the brain, infection, increased pressure within the chambers (ventricles) of the brain, radiation or trauma to the pituitary gland can cause hypothyroidism.
What are some of the possible effects of hypothyroidism?
Signs and symptoms of hypothyroidism may include decreased growth rate, weight gain, decreased activity energy, low body temperature, dry skin, cold intolerance, constipation, tiredness, puffiness of the face, mild anemia, slow speech and delayed sexual maturation. Occasionally premature sexual maturation may occur.
How is acquired hypothyroidism diagnosed?
Hypothyroidism usually is diagnosed by learning about the child’s symptoms and by giving the child a thorough physical examination. Blood test may include thyroid hormones (T3 and T4), TSH, thyroid antibodies, and thyroid binding globulin (TBG). If the blood tests are abnormal the doctor may order special X-rays. An ultrasound of the thyroid gland may also be obtained. Radioactive Iodine Scan (RAI) uses dye and X-rays to determine the presence and function of the thyroid gland. A bone age X-ray of the left hand and wrist may be done to see how your child’s bones are growing.
How is acquired hypothyroidism treated?
The treatment of hypothyroidism is simple and effective. Your child will be given medicine, called L-thyroxine (also known as levothyroxine, Levoxyl, Synthroid), in the form of a tablet to replace the thyroid hormone. Lthyroxine is the same as T4. All of these preparations are human Lthyroxine. They are immediately converted by enzymes in the body to T3, providing just the right mix of T4 and T3 to regulate metabolism. We do not prescribe animal thyroid hormone extracts, as they do not provide the body with consistent, reliable thyroid hormone levels to mimic the natural secretion of thyroid hormones. It is very important that the medication be taken every day, preferably at the same time. A pillbox may be helpful to keep track of the pills that are given. Despite what the pharmacist may tell you to the contrary, you are encouraged to make up any missed doses by taking extra pills all at once. Do not take it at the same time as any iron or calcium supplements, or any soy products. Be sure you have the prescription filled before you are completely out of medication to avoid missing doses. Always keep your doctor informed of your child’s status. You may see the following signs if your child is getting too much thyroid medicine: poor sleeping, tremors (shaking), weight loss, irritability, palpitations, diarrhea, or excessive hunger. If your child is not getting enough thyroid medication you may see: sleeping for long periods of time, constipation, dry skin, excessive weight gain, or decreased energy/activity. If you notice these symptoms, contact your doctor. The dose may need to be adjusted. Never adjust the dose of thyroid medication yourself; a blood test will be necessary first.
When should the doctor see my child?
Your child needs to be seen at our office for exams, growth checks and blood tests to make sure the correct amount of thyroid medication is being taken. Depending upon your child’s age, and stability of thyroid hormone levels, we usually see children with acquired hypothyroidism every 3 – 12 months. Remember that you will also need to continue to follow up with your child’s primary care physician for routine medical care.
What is the future for my child?
With proper treatment and follow-up your child has a very good prognosis for normal development of all body systems. It is important to follow your doctor’s orders for giving thyroid replacement medication.
